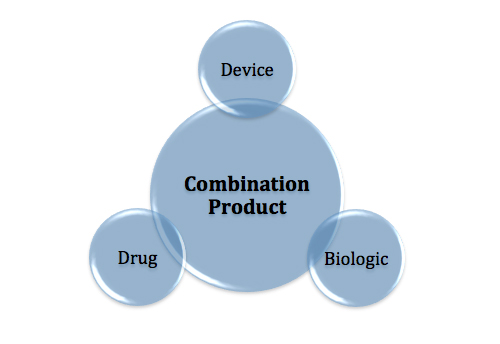
As the convergence of drug and device products continues in medtech and the regulatory requirements for combination products are more clearly defined, companies must be familiar with best practices to streamline new product submissions. The recent trend of pharmaceutical companies acquiring medical device start-ups to supplement their R&D pipeline and expand combination product innovations continues. Teva Pharmaceuticals recently acquired Gecko Health to provide a device platform for many of its respiratory therapies, an example of the pharmaceutical industry recognizing the value in novel delivery platforms that can expand target users and drive increased adoption. FDA has closely monitored these activities and established the Office of Combination Products (OCP) along with new rules and guidance that establish a framework for combination product manufacturers. This article focuses on two key aspects to consider when preparing a regulatory submission to the FDA for your combination product.
1. Classify Your Drug or Device Appropriately to Set the Tone for Your Development and Application
When deciding whether your drug-device combination product will be regulated as a device or a drug, the product’s primary mode of action (PMOA) must be determined. By this point, you’ve hopefully established that your dual product is, in fact, a combination product per 21 CFR 3.2 (e).
As defined in the Federal Register, the PMOA is “the single mode of action of a combination product that provides the most important therapeutic action of the combination product”. For example, in the case of most drug-coated stents, the primary contributor to the intended use of opening vasculature is the device. The drug is primarily an aid that helps to keep a lumen patent via chemical means. However, most drug-delivery injection pens have PMOAs of a drug since the device (the pen) acts primarily as the delivery vehicle.
503(g)(1) of the FD&C describes that the lead agency in charge of combination products depends on the PMOA. In the case that the PMOA is a drug, the full application is sent to CDER, whereas if the PMOA is a device, CDRH becomes the lead agency. However, inter-agency cooperation is necessary to ensure that each respective branch reviews the appropriate matter that represents their subject matter expertise.
Having trouble determining whether your product is a device or a drug? The FDA’s Request for Designation (RFD) process provides a mechanism in which the agency issues a letter of designation that becomes a binding determination with respect to classification and/or center assignment. The RFD process is further explained in a guidance document entitled “How to Write a Request for Designation”, published in 2011.
2. Design History Files Are Expected for Devices as Combination Products – even if the product is submitted in a drug application
Preparing the regulatory strategy for a combination product can be a tricky endeavor. The key-determining factor is once again, PMOA. If the PMOA is a drug, the submission is expected to follow typical drug submission routes suh as those mandated in Investigational New Drug (IND) and New Drug Application (NDA) submissions using 505(j), 505(b)(1), 505(b)(2) as guidance. If the product is considered a device, the manufacturer is expected to submit the product as a 510(k) or PMA—the typical device pathways. Determining a combination product’s regulatory submission is in itself an entire article so let’s focus on something that all submissions must have (even the drug applications): a design history file (DHF) describing the device.
In the case of device applications, the device is clearly a focal point, and there is significant available guidance on preparing 510(k)s and PMAs. However, how in depth does the device portion of a Drug PMOA combination product submission need to be? Because of the nature of the submission, the primary focal point of the submission—from the perspective of FDA’s critical review—will most often be the drug information, including identification, pharmacokinetics, pharmacodynamics, dosing, stability and other information that characterizes the safety and efficacy of the API and the drug product. However, the device development is also reviewed, chiefly to ensure that functional and performance expectations are met and don’t compromise the therapeutic efficacy of the drug being delivered.
So, what is the expected depth and breadth of a DHF as it relates to a drug submission? This is a controversial topic within the medtech industry, and it does not have a clear-cut answer. Let’s first examine the FDA’s guidance on combination products (January 2015) and assume that an NDA is being developed, which would represent the worst case in terms of requiring the most documentation from a manufacturer. In the guidance, the FDA indicates that even for investigational devices (in this case, an IND, which often will precede an NDA), the constituent part of the regulations will still apply. Interpretation? The device requirements in a combination product submission are the same as if submitting the device as a standalone product. Thus, 21 CFR 812 Investigation Device Exemption requirements, which define “what’s needed from a quality management system perspective for investigational medical devices”, apply. This regulation states that cGMPs are not required—except design controls (21 CFR 820.30).
The next step, both for the IND and for subsequent support of an NDA, is determining “how much is enough?” when it comes to building the case for safety and efficacy of the device (from a design controls perspective). The answer, in typical consultant fashion, is that it depends! Let’s focus on only a few of the key elements of 21 CFR 820.30 that should be a focal point of the DHF in a drug device submission:
- Design and Development Planning. A design and development plan is typically required in order to provide proper context and scope to the extent of device development. A key determination in this phase is establishing the rationale for the design controls elements that are implemented, those that are not, and rationale for these decisions. In combination product submissions, it is particularly important to identify development partners, including contract manufacturers, developers and vendors that support design elements. Design and development planning should also describe plans for testing the device. Will be it tested as a base product (without a drug?) or in combination with the drug, for critical tests like stability, functionality and performance testing? Will human factors or usability testing per IEC 62366-1 be in scope? Usability and human factors work is often requested by regulators to support combination product applications; proving that device use errors in injection pens that compromise delivery (under-dosing/ overdosing), for example, is critical towards establishing the therapeutic benefit of the drug being delivered.
- Design Inputs. As a general rule, the more complexity and risk that is associated with the device, the more design inputs will be required to adequately characterize it. In combination products, design input documentation should cover key user needs and key interface requirements between the device and drug. Common requirements would include: Extractables and leachables in a drug container, drug delivery volumes, rates and flows in injection or inhaler products, and mechanical integrity in most products where a toxic drug is contained.
- Design Verification. The approach to design verification is very similar to that of design inputs. The goal in design verification is to demonstrate that the device doesn’t introduce a safety issue into the overall product, nor does it compromise therapeutic performance of the drug or impart negative characteristics onto the drug, such as biological residues that can lead to infections. Testing should be conducted as a combination product as much as possible. This rules out potential adverse issues with the device and drug operating in concert in downstream clinical trials or prior to commercialization.
Overall, the depth and breadth of the DHF for a device in a drug-device submission should be scaled to the complexity and risk associated with the product. As a last piece of information: If the product is based on well-established predicates or comparable competitor products, the rigor and extent of the DHF could potentially be reduced. Having supported many combination product submissions, I can summarize best practices by reminding manufacturers to justify the scaling and extent of the device constituent of a drug device product.