
The mission to bring meaningful innovation to market and improve patient lives is paired with the requirement that such innovations are held to the highest quality. There were 70 class I U.S. medical device recall events in 2022, a category that the FDA reserves for problems that may lead to serious death or injury. Class I recall events are at a 15-year high, up from an average of 47 recalls annually over the past five years. We must do better.
Recalls pose a significant challenge to medical device manufacturers. The most frequent reasons for Class I recalls, as cited in the FDA Medical Recall report, were related to quality system regulation including:
- Device and software design
- Non-conformance
- Process controls
The Importance of Traceability
Medical device manufacturers are required to follow stringent global quality system processes with traceability to ensure patient safety in an evolving regulatory environment. Design controls are part of the quality system requirements and are a set of quality practices and procedures that control the design process to assure the device meets user needs, intended uses and specified requirements. It may seem easy to use a simple spreadsheet to document and manage design controls—user needs, design inputs, design outputs, design verification, design validation—yet this creates a fragmented process and a paper trail that will delay the development cycle.

Design traceability is documenting the relationships between layers of design to help systems engineers better manage requirement changes during the product design and development process. The evolving nature of designing a medical device requires a system that supports continuous iteration of the design and seamless handoffs between teams. As a device goes through testing, issues are found, designs are modified and documentation is updated. This requires a process that goes beyond documenting and tracking changes; it must effectively connect people, processes and data. Manually tracking design controls on paper is bound to cause errors due to requirements not being properly linked to the design or test cases leading to recalls or other corrective actions.
To deliver optimum value, product traceability should have forensic-level probability and the ability to track the product progress from its original design to development and post-market use including all changes thereafter.
Digital Continuity Beyond CAD & PLM
Moving from a document-based approach to a data-driven approach ensures an organization can confidently access accurate data to enable informed decision making. The connection of product data across a company’s engineering, manufacturing, supply chain and service functions means people spend less time searching for information. Rather they have access to a system with timely, trustworthy and accurate data and insights. Digital continuity across the value chain includes the use of product data to produce digital work instructions on the shop floor and artificial intelligence to analyze quality trends.

Nonconformance can have a significant impact on patient safety leading to increased costs, regulatory penalties, and recalls. A nonconformance occurs when a product does not meet its specified requirements, which can occur at both the product and process level. Documenting and responding to a nonconformance is a crucial part of a quality management system for medical device manufacturers. Handling nonconforming products at the serial number level by using manual methods has high risk for potential error including identifying which units are still in the warehouse, which are still on the factory floor in WIP (work in progress), and how many units have been shipped to customers. A nonconformance can be a result of many varied factors including changes at the supplier, errors in the manufacturing process, design defects, poor quality materials, or user error. One of the most significant causes of process nonconformance on the shop floor can be human error or frontline personnel deviating from work instructions. This may be due to inaccurate, unclear, or outdated processes. Data linkage and the use of product data to update work instructions and generate intelligent digital mock-ups ensures quality and accuracy at every workstation.
The addition of cutting-edge technologies such as intelligent machine vision, AI and deep learning can connect engineering to production on the manufacturing shop floor to ensure repeatable right-first-time operations. Manufacturers can develop algorithms of deep learning that spot the presence of defects, or other anomalies during the manufacturing process as well as the products to help workers on the shop floor. Deep learning and machine vision can play crucial roles in transforming the manufacturing industry by enhancing quality control, automation, and productivity.
Intelligent Ecosystems To Drive Innovation
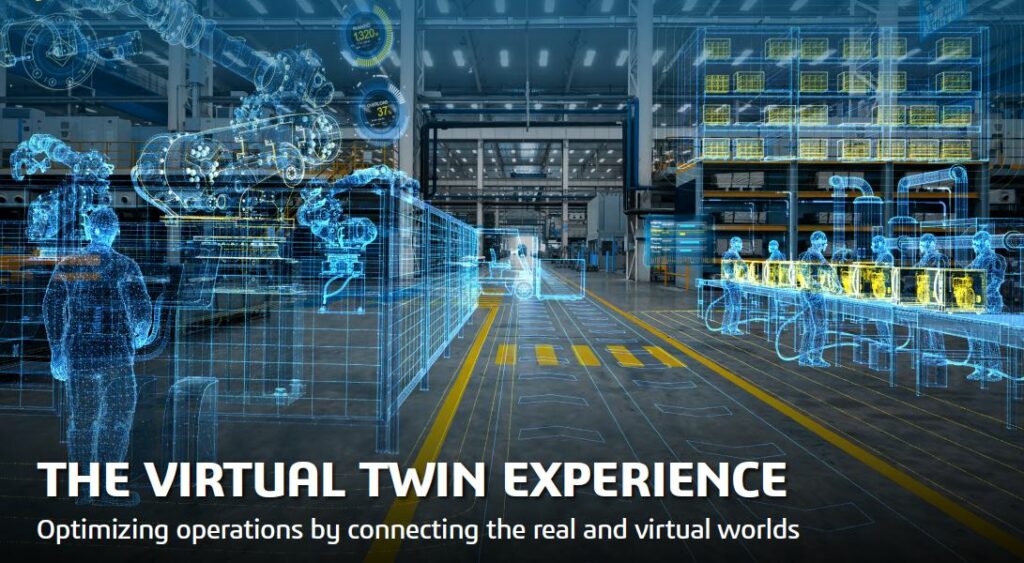
The pace of medical device innovation will be fueled by those that have figured out how to create more agile and resilient organizations leveraging flexible and extensible technologies. This next phase of medical device innovation will lean on tried and tested technologies from adjacent industries to invent the next generation materials and products. While science will outpace regulations, pushing the scientific boundaries will lead to the next generation of medical device innovation. An existing linkage that will drive MedTech innovation is the adoption of virtual twins across the value chain. This data linkage between historically disparate systems in design, manufacturing, service, and post-market surveillance creates new opportunities for innovation.
The use of computational modeling & simulation (CM&S) to make design decisions is not a new concept. However, the science of simulation has advanced in silico studies with advantages over other forms of design testing, including bench and animal studies. These advantages include the ability to integrate patient-specific data and conduct parametric and statistical analyses in a controlled environment with the ability to test edge cases that were historically impossible to study. Creating virtual patient cohorts to model the interaction between devices and humans earlier in the design phase will answer design questions that have historically only been answered later in the design process and sometimes only discovered once a device is already in the market in a clinical trial. Proactive testing of unique patient anatomies, anomalies, and failure modes creates more certainty in the design performance and reliability much earlier in the design process. In addition, the advancement of American Society of Mechanical Engineers (ASME) verification and validation (V&V) 40 guidelines and procedures outline a framework to help practitioners assess the relevance and adequacy of completed V&V activities to establish credibility of a computational model.
Intelligent computational modeling can also be extended to the manufacturing shop floors across many industries including MedTech. In this age of technology, access to equipment and techniques with intelligent image processing capabilities enables the use of machine vision across the production process to detect imperfections that are invisible to the human eye. For example, machine vision can detect nonconformance in products including the symmetry of a component or the markings of a product label. The data linkage between engineering and shop floor operations can make digital models accessible on the shop floor to create real-time, contextualized image-guided work instructions.
Some manufactures are using advanced artificial intelligence systems to connect data silos across functions all the way to the patient. MedTech manufacturers have both structured and unstructured data that can be used to train intelligent systems for predictive, reactive and corrective actions. Deep learning models are able to detect inefficiencies and suggest processes that can be optimized to increase the efficiency of production and minimize the amount of waste, while enhancing the ability to see things that may cause recalls down the line. When a supplier changes a component specification without notifying the device manufacturer, artificial intelligence can be trained to identify deviations in specifications. By leveraging AI, the manufacturer can proactively identify nonconformance.
As medical devices become more complex with integrated systems, manufacturers are adopting intelligent ecosystems that can future-proof the value chain. A recent Deloitte survey of 100 executives from large MedTech companies across the United States, Europe and Asia identified three business functions where leaders are using digital technologies to maximize impact[1]:
- Innovation & Product Development
- Manufacturing & Supply Chain
- Marketing & Commercial
Across innovation and product development, MedTech companies are investing in digital clinical trials. As this trend continues, we will see the growth of in silico and digital clinical trials across many functions including engineering and clinical trials. Within manufacturing and supply chain, building smart factories was by far the No. 1 use case. There is no doubt that MedTech is moving towards a more digital future.
References:
[1] Has Medtech Entered the Era of Digital Innovation?
Ask the Expert is a sponsored content program. MedTech Intelligence writers and editors were not involved in the creation of this content. Publishing of this content by MedTech Intelligence is not an endorsement of the content, products or services mentioned herein.
This post is sponsored by:







