For more than a decade, robotic-assisted surgery has been used for a variety of procedures, from total hip replacement to bariatric surgery to coronary artery bypass grafting. One of the challenging areas of exploration has been soft tissues due to the unpredictable characteristics of the tissue.
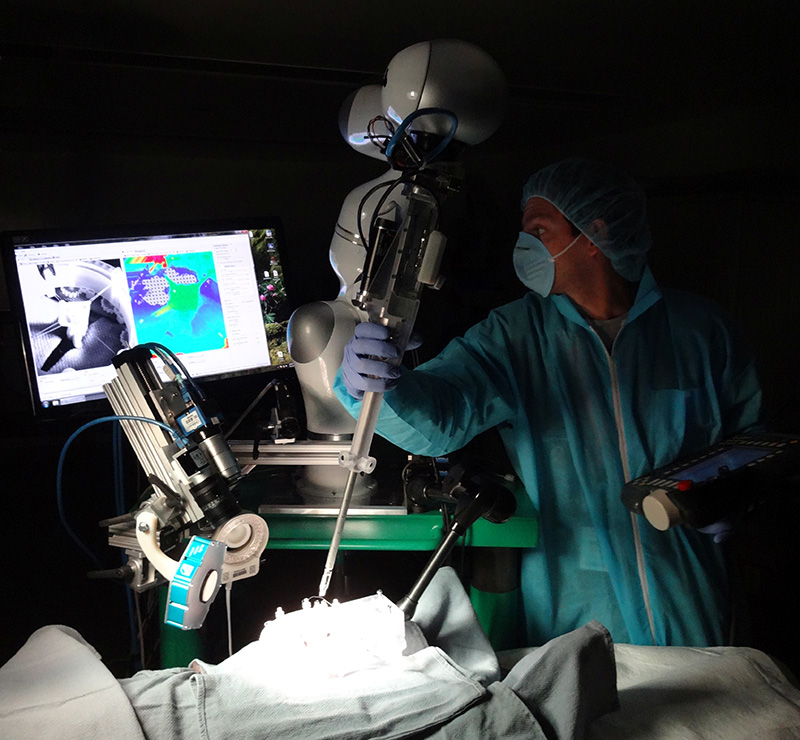
Surgeons at the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National Health System recently have shown that robotic-assisted surgery of soft tissue may improve clinical outcomes and could outperform traditional clinical techniques. Their study was published in Science Translational Medicine, and involved a comparison of the effectiveness of robotic technology developed at Children’s National, called Smart Tissue Autonomous Robot (STAR), to current available procedures.

“Until now, autonomous robot surgery has been limited to applications with rigid anatomy, such as bone cutting, because they are more predictable,” said Axel Krieger, Ph.D., technical lead for smart tools at Sheikh Zayed Institute in a press release. STAR was designed to address the difficulties of working with soft tissue on a robotic platform. It uses a tracking system that has near infrared florescent markers and 3-D plenoptic vision to generate 3-D images, which allows surgeons to track tissue motion and any changes that occur with the tissue during surgery. “By using novel tissue tracking and applied force measurement, coupled with suture automation software, our robotic system can detect arbitrary tissue motions in real time and automatically adjust,” Krieger said.
The study was conducted on both inanimate porcine tissue and living pigs, and involved linear suturing and end-to-end intestinal anastomosis. The study compared supervised autonomous robotic procedures using STAR with surgery performed by experienced surgeons and robotic-assisted surgery with the daVinci Surgical System, and found the STAR procedures to be superior on both the static porcine tissues and living pigs. However, the manual control surgery took only eight minutes, compared to 35 minutes using STAR technology (yet the researchers said that this is comparable to the average time to complete laparoscopic anastomosis at 30 to 90 minutes).
According to Peter Kim, vice president and associate surgeon-in-chief at the Sheikh Zayed Institute, the next step is to make the tools even smaller and refine the sensors in order to expand the application potential for the STAR system. If the institute finds the right partner, it’s possible that the technology could be brought into the clinic within two years.