Optimize Combination Products: Select a Drug Delivery Device that Meets User Needs
Pharmaceutical companies invest substantially in the development of new, innovative therapies. However, while they spend considerable time and money developing a safe and efficacious drug, many companies do not make a concomitant investment in the development of an equally safe and effective drug delivery device. The choice of device might be far from an afterthought, but it has the potential to become a late-stage, somewhat rushed initiative.
In haste to get to market, some pharmaceutical companies select a device without fully considering whether intended end-users—the intended patient population—can use the device safely and effectively. Choosing a suboptimal and arguably flawed device can induce user interaction problems, which can lead to a failed summative (i.e., validation) usability test and hinder a company’s ability to get an important drug to market.
Given this pattern, pharmaceutical companies are well-served to select a device that is not only compatible with the drug, but that is also compatible with and carefully matched to the intended users and the associated use scenarios and critical tasks. Ensuring alignment is bound to increase the likelihood that users can interact with a given drug-device combination product safely and effectively, which boosts the likelihood of a successful human factors validation effort.
Device Selection Considerations
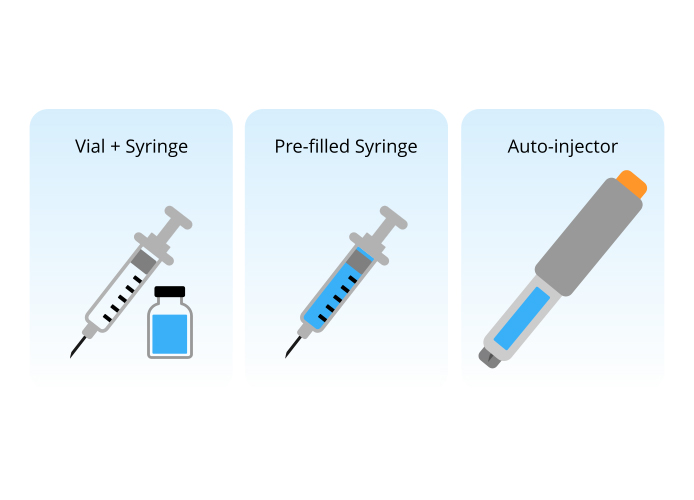
In many cases, multiple types of devices might be suitable to deliver a particular drug. For example, a drug intended for subcutaneous injection could be delivered using a patch pump, syringe and vial, pre-filled syringe, pen-injector, or auto-injector. Similarly, a metered-dose inhaler, dry-powder inhaler, or nebulizer might all be appropriate delivery devices for medication delivered via the lungs. When multiple device options exist, companies should carefully consider user needs as a key selection criteria. We describe some device selection considerations below.
User Impairments
Pharmaceutical companies should take the steps necessary to define users’ physical and cognitive capabilities (and, accordingly, limitations) and the potential impact on their ability to use a drug delivery device safely and effectively. Impairments that might affect whether intended users can use a given device and considerations of how to mitigate include the following:
Manual dexterity impairments. Assess whether users experience challenges working with their hands. Manual dexterity impairments, such as arthritis, neuropathy (numbness), muscle weakness, range of motion limitations and tremor, can all affect a person’s ability to handle a device properly. Subsequently, device features may be optimized—if there is design flexibility—to accommodate particular user impairments. Alternatively, one existing device might be better at accommodating the impairments.
For example, some individuals with rheumatoid arthritis might not have the fine motor control to grip and stabilize a narrow device, such as a syringe, but they can securely hold and manipulate a longer and wider device, such as an auto-injector.
Involuntary hand movements, such as those that might be associated with Parkinson’s Disease, Essential Tremor, and even stress or nervousness, is another manual dexterity impairment that can pose device interaction problems. The condition might complicate use of an injection device that requires users to hold the needle in the skin for several seconds. In fact, this task would be quite challenging for someone with shaky hands. Considering this impairment, the quality and safety of user-device interactions might be improved by a device, such as an adhesive patch pump, that does not require users to manually hold the device in place during drug delivery.
Visual impairments. Consider whether users have condition- or age-specific visual impairments. Conditions such as retinopathy, cataracts, glaucoma, or color blindness can cause user interaction problems if the device does not accommodate such impairments. Accordingly, a device that does not rely on users to read and interpret small text or visual cues (e.g., thin, small graduation marks on a syringe) might be the best choice.
Cognitive impairments. Assess whether users experience any cognitive impairments, such as memory loss, learning challenges, or difficulty concentrating that might hinder their interactions with a drug delivery device. For example, some people with Multiple Sclerosis are unable to reliably recall and execute a multi-step process, such as manually reconstituting (i.e., mixing) a drug comprised of diluent and powdered components contained in separate vials. However, people with Multiple Sclerosis might be more consistently be able to complete a simpler and shorter, three-step process without difficulty.
Continue to page 2 below.
Drug Administration Attributes
A drug’s intended use, including the frequency with which the drug is administered and the urgency of drug delivery, should also be driving factors in device selection. Users’ prior experience using such devices is also a key consideration. We describe these drug administration attributes and our experience below.
- Frequency. The best drug delivery device might differ based on use intervals (e.g., daily, weekly, monthly). For a drug delivered daily, users will likely value a device that has few set-up and administration steps, delivers drug in seconds, and minimizes disruption of their daily routine. That said, users are likely to become highly skilled at using a device they use daily, suggesting that they will eventually become adept at using a more complex device. By comparison, a device intended for more seldom, monthly drug administration should probably have a limited number of use steps (two to four), recognizing that users interact with the device infrequently and might need to intuit the steps if they cannot recall a multi-step administration process.
- Urgency. Drugs that must be delivered urgently, such as Epinephrine to someone experiencing anaphylaxis as a reaction to an allergen, should be paired with a device that facilitates rapid use, noting that near-immediate medication delivery is essential to ensure effectiveness. These users do not have time to read instructions or study the device to figure out how to operate it. Furthermore, users responding to an emergency can be stressed, have shaky hands, and be unfamiliar with the device. As such, emergency-use devices must enable quick—and safe and effective—use, regardless of factors that might hinder optimal use. Characteristics that facilitate rapid, successful drug delivery include a device with few use steps, no assembly, large non-slip grip surfaces, as well as conspicuous on-device instructions describing and/or illustrating key steps.
- User experience with the device. As previously suggested, some drug delivery device users might not have prior experience with a given device. For example, a passer-by might have to administer Epinephrine to a stranger experiencing a severe allergy attack in a park. Features such as clearly marked hazards (e.g., needle end), orientation cues indicating how to hold the device, and prominent instructions that convey the route of administration (e.g., subcutaneous injection, nasal spray), can all facilitate correct use by untrained and inexperienced users.
Device Characteristics
Users often express the need for specific device characteristics (e.g., highly portable) that will maximize the convenience of fitting the drug delivery device into their lives. Several device user interface characteristics should be considered during device review and selection.
- Portability. Devices that users must carry with them at all times, such as a rescue inhaler used to treat an asthma attack, should be optimized for such use. Portability rests on a device’s compactness, relatively low weight, durability, temperature stability, and safeguards against accidental actuation due to rough handling (e.g., storage in a child’s backpack that gets tossed around). If a device is truly portable, it is more likely the user will have it with him or her when the medication is needed.
- Discreetness. Some users will prefer to use a device with which they can interact discreetly—without drawing undue attention, such as during use in a restaurant, theater, classroom, athletic venue, etc. For example, some people with diabetes appreciate a device that enables them to deliver insulin during a public dinner without others noticing.
- Workload. Administering medication routinely can disrupt users’ lives in profound or insidious ways that equate to “treatment burden.” The extent to which users accept drug delivery devices with high treatment burden varies. The device selected for users who already have many treatment options (e.g., people with diabetes) should reduce treatment burden (e.g., make treatment faster, easier, less painful, less frequent). In contrast, it might be acceptable to select a device that that is somewhat inconvenient, intrusive, and/or time-consuming to use if the end-users have limited or no treatment options (e.g., people with a very rare condition) because it is their only option for treating or managing the symptoms of their condition.
Conclusion
Companies are well served to follow a drug delivery device selection process informed by user needs, capabilities and preferences. The process might lead them to an optimal device that users can easily integrate into their lives, ensuring safe and effective use as well as good compliance with the given therapy regimen. In lieu of a good selection process, companies might face an uphill battle when it comes time to validate their chosen drug delivery device. As such, a user-centered approach to device selection/design is a benefit to the end-users while also being good for business.
In a follow-up article, we will provide some advice regarding how companies can exercise due care when evaluating off-the-shelf drug delivery devices, assessing the extent to which human factors and an assessment of users’ needs was performed during device development.